Non-communicable diseases in disasters and emergencies: the elephant in the room
25 Jun 2025
Written by Dr Bhavya Balasubramanya
Reviewed by Dr Maya Cherian
Background
Non-communicable diseases (NCDs) are a group of chronic conditions that are generally slow in progression, long in duration, and rarely completely curable. These conditions result from interactions between genetic, physiological, environmental and behavioural factors. NCDs include a wide range of conditions such as diabetes, cardiovascular disease, chronic respiratory disease, cancers, kidney disease, genetic disorders, mental health conditions, injury, and many more.
From a societal perspective, NCDs have a direct impact on health and well-being, productivity, socioeconomic costs and mortality. Globally, NCDs represent both a current and future public health challenge.
Global burden of non-communicable diseases
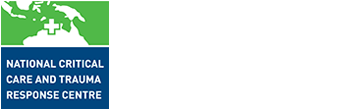
NCDs affect people of all ages worldwide, causing 43 million deaths each year and accounting for 71% of all global deaths. More than three-quarters of these occur in low- and middle-income countries. Cardiovascular disease is the leading cause of NCD-related deaths, followed by cancers and chronic respiratory diseases. There has been an increasing trend in morbidity caused by NCDs over the past three decades (Figure 1 and 2) with cardiovascular disease, cancers, chronic respiratory diseases and diabetes accounting for the top four causes (Figure 3).
Figure 1: Global burden of disease 1990 – 2021. Our World in Data.
Figure 2: Global burden of NCDs by type over 3 decades. Our World in Data.
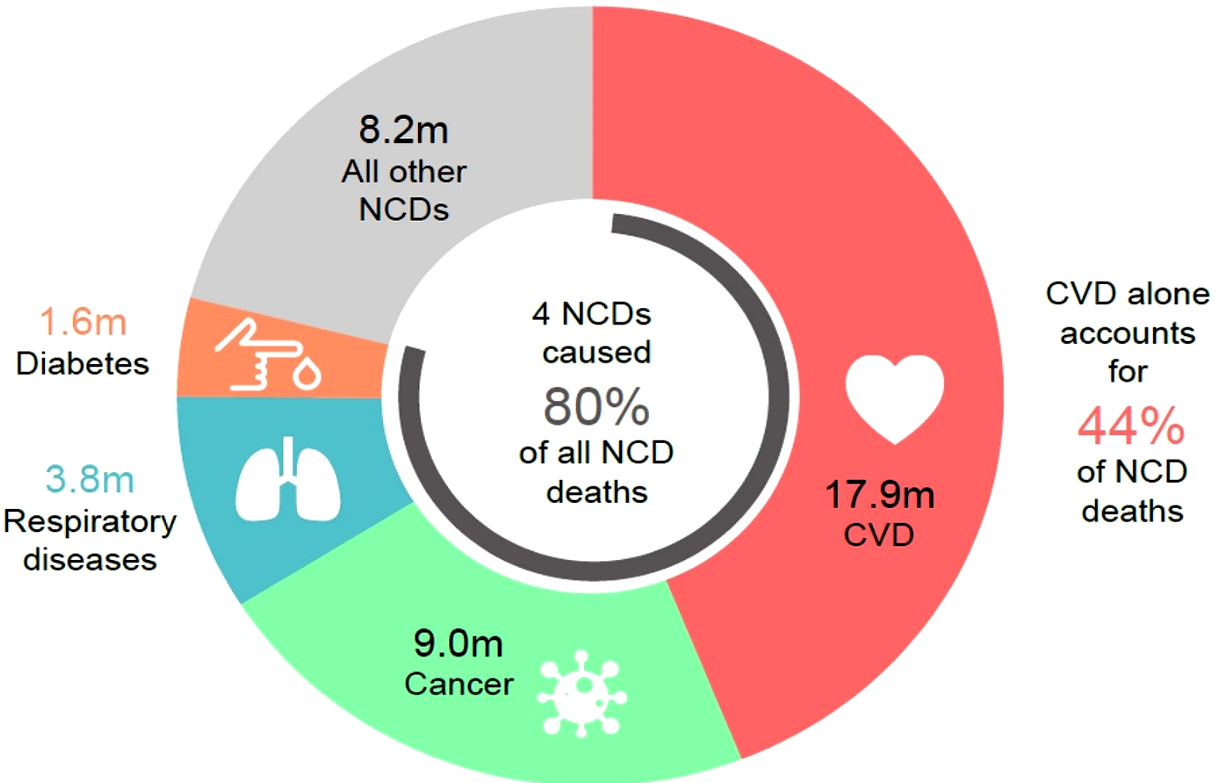
Figure 3: Global annual deaths by key NCDs. World Health Organization.
Children, adults and the elderly are all vulnerable to NCD risk factors (Figure 4) yet an estimated 80% of these diseases are preventable.
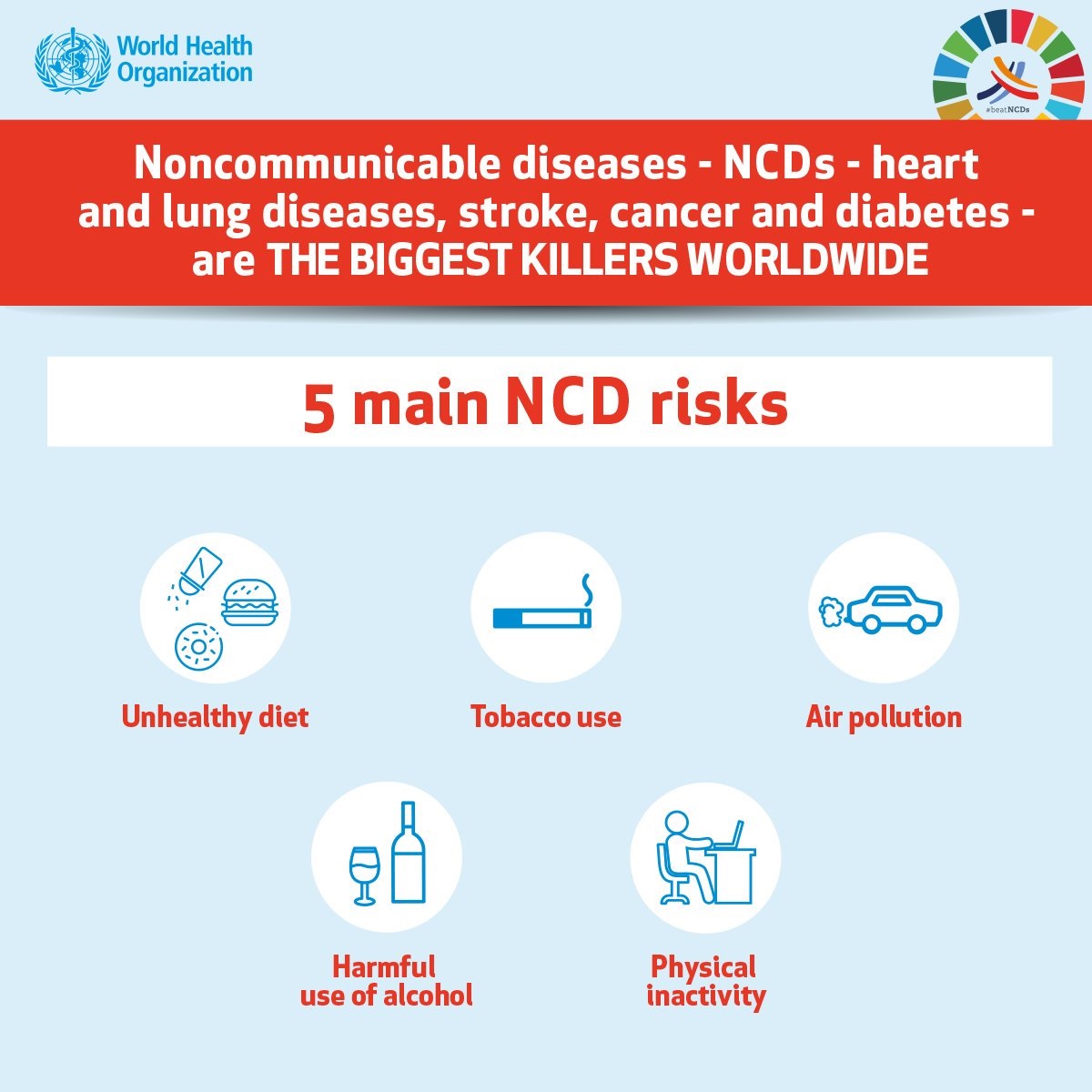
Figure 4: Five main risk factors for NCDs. World Health Organization.
NCDs in emergency and disaster settings
Disasters, conflicts, and mass displacement disrupt access to healthcare, increasing vulnerability among people with NCDs, disabilities, or injuries.
Impact of disaster on people living with non-communicable diseases
Addressing NCDs in emergencies
Traditionally disaster response has heavily focused on communicable diseases, injury and trauma. However, the time has come for a paradigm shift. With the global rise in disasters and the prevalence of people suffering from chronic diseases, there is a need to strengthen emergency preparedness, response and recovery efforts for patients living with chronic diseases.
In 2023, the World Health Organization (WHO) Regional Committee for the Eastern Mediterranean endorsed a regional framework to address NCDs in emergencies. The framework outlines a set of strategic, actionable interventions that align with the phases of an emergency management cycle (Figure 5).

Figure 5: WHO framework to address NCDs in emergencies. World Health Organization.
Preparedness phase
To mitigate the risk that disasters pose to people living with non-communicable diseases (PLWNCD), a multi-sectoral approach is required, which may include cross-cutting disaster strategies such as:
- Integrating an NCD emergency plan within the national preparedness plan. Disaster response strategies should explicitly address the needs of people with NCDs, including access to medications, healthcare services and mental health support
- Implement robust surveillance systems to collect data on NCDs and related risk factors to help map vulnerabilities within communities
- Ensure availability and access to contingency funding to meet NCD needs during an emergency response, including financial protection mechanisms for PLWNCD
- Investing in resilient healthcare infrastructure to ensure continued access to care during and after disasters
- Health promotion: public education on the impact of disasters on NCDs and the importance of NCD management plans in disaster-prone areas can help reduce the risk of adverse outcomes.
Response and recovery phase
- Activation of national mechanisms to secure NCD medicines and supplies during emergencies, for example through NCD emergency kits
- Assign an NCD focal point within the emergency response team
- Continue to strengthen strategies established during preparedness phase
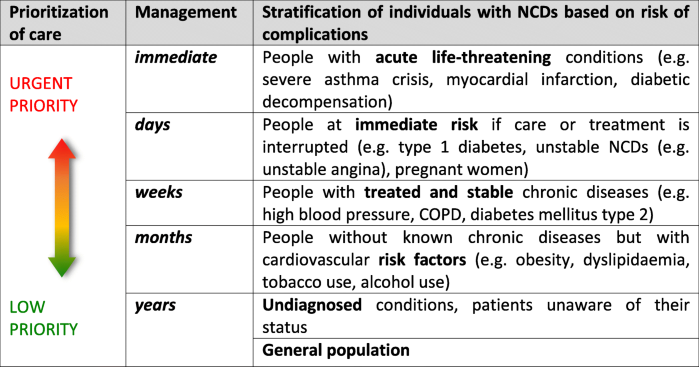
The WHO Emergency Medical Teams 2030 Strategy calls for strengthening global health system resilience, while the United Nations Sendai Framework for Disaster Risk Reduction 2015-2030 aims to minimise disruption to basic health services. Figures 6 and 7 are suggested models for operational prioritisation for NCD care during the response and recovery phases of an emergency:
AUSMAT’s deployment to Vanuatu in 2024 following a magnitude 7.2 earthquake is a prime example of how emergency medical teams (EMTs) can support NCD care. AUSMAT assisted the renal dialysis unit by providing vascular access for dialysis, assessing and advising on water quality, and repairing the hospital’s oxygen concentrator. AUSMAT also has guidelines for the clinical care of PLWNCDs during emergencies.
AUSMAT’s experience during Typhoon Haiyan in the Philippines in 2013 where surgical patients with diabetes were managed in a field hospital, led to the development of a model for acute NCD care following sudden-onset disasters. This model highlights the importance of addressing NCDs as a key component of disaster response and recovery.
As the frequency of disasters increase and response strategies evolve, the integration of NCDs into emergency planning is essential. NCDs should be addressed at all stages of the emergency management cycle.
References
- Bausch FJ, Beran D, Hering H. et al. 2021. Operational considerations for the management of non-communicable diseases in humanitarian emergencies. Conflict and Health. doi:10.1186/s13031-021-00345-w
- Dain K. 2018. Challenges facing global health networks: the NCD Alliance experience. Comment on “Four challenges that global health networks face.” International Journal of Health Policy and Management 7(3):282–285. doi:10.15171/ijhpm.2017.93.
- Ghazanchaei E, Khorasani-Zavareh D, Aghazadeh-Attari J, Mohebbi I. 2021. Identifying and Describing Impact of Disasters on Non-Communicable Diseases: A Systematic Review. PubMed Central. doi:10.18502/ijph.v50i6.6413
- Global Alliance for Chronic Diseases. 2025. Non-communicable diseases.
- McDermott KM, Hardstaff RM, Alpen S, Read DJ, Coatsworth NR. 2017. Management of Diabetic Surgical Patients in a Deployed Field Hospital: A Model for Acute Non-Communicable Disease Care in Disaster. Prehospital and Disaster Medicine 32(6):657-661. doi:10.1017/S1049023X17006707
- Roser M, Ritchie H, Spooner F. Published 2016, updated 2024. Burden of disease. Our World in Data.
- United Nations Office for Disaster Risk Reduction. What is the Sendai Framework for Disaster Risk Reduction?
- World Health Organization. 2023. Emergency Medical Teams 2023 strategy.
- World Health Organization. 2024. Alcohol, Drugs and Addictive Behaviours.
- World Health Organization. 2024. Addressing non communicable diseases in emergences: a regional framework for action. WHO-EM/NCD/154/E.
- World Health Organization. 2024. NCDs in emergencies.
- World Health Organization. 2024. Noncommunicable Diseases.
- Yeung C. 2025. AUSMAT Spotlight on Mitchell Bourke: from repairs to recovery in Vanuatu’s earthquake response. National Critical Care and Trauma Response Centre.
- Yeung C. 2025. United in support: AUSMAT’s response to Vanuatu’s earthquake. National Critical Care and Trauma Response Centre.