AUSMAT and Pacific EMTs: emergency blood banking skills for surgical readiness
06 Oct 2025
Written by Erika Lu
In a powerful display of regional collaboration and clinical excellence, 22 members of the Australian Medical Assistance Team (AUSMAT) joined forces with nine emergency medical professionals from across the Pacific to sharpen their skills in disaster surgery and field anaesthetics.
Held as part of the National Field Exercise, the four-day AUSMAT Surgical Team Member Course brought together participants from Fiji, Papua New Guinea, Samoa, the Solomon Islands, Vanuatu, and Australia. They trained side-by-side in the fully deployable AUSMAT Emergency Medical Team (EMT) Type 2 Surgical Field Hospital — a compact, mobile facility designed to meet and exceed the World Health Organization (WHO) EMT minimum standards.

AUSMAT member and Medical Scientist Leanne Jones from the National Critical Care and Trauma Response Centre (NCCTRC) explained, “The EMT Type 2 field hospital includes a state-of-the-art laboratory capable of diagnostics, blood transfusion services and infection control in austere environments. It enables advanced point-of-care testing, blood banking and molecular diagnostics.”
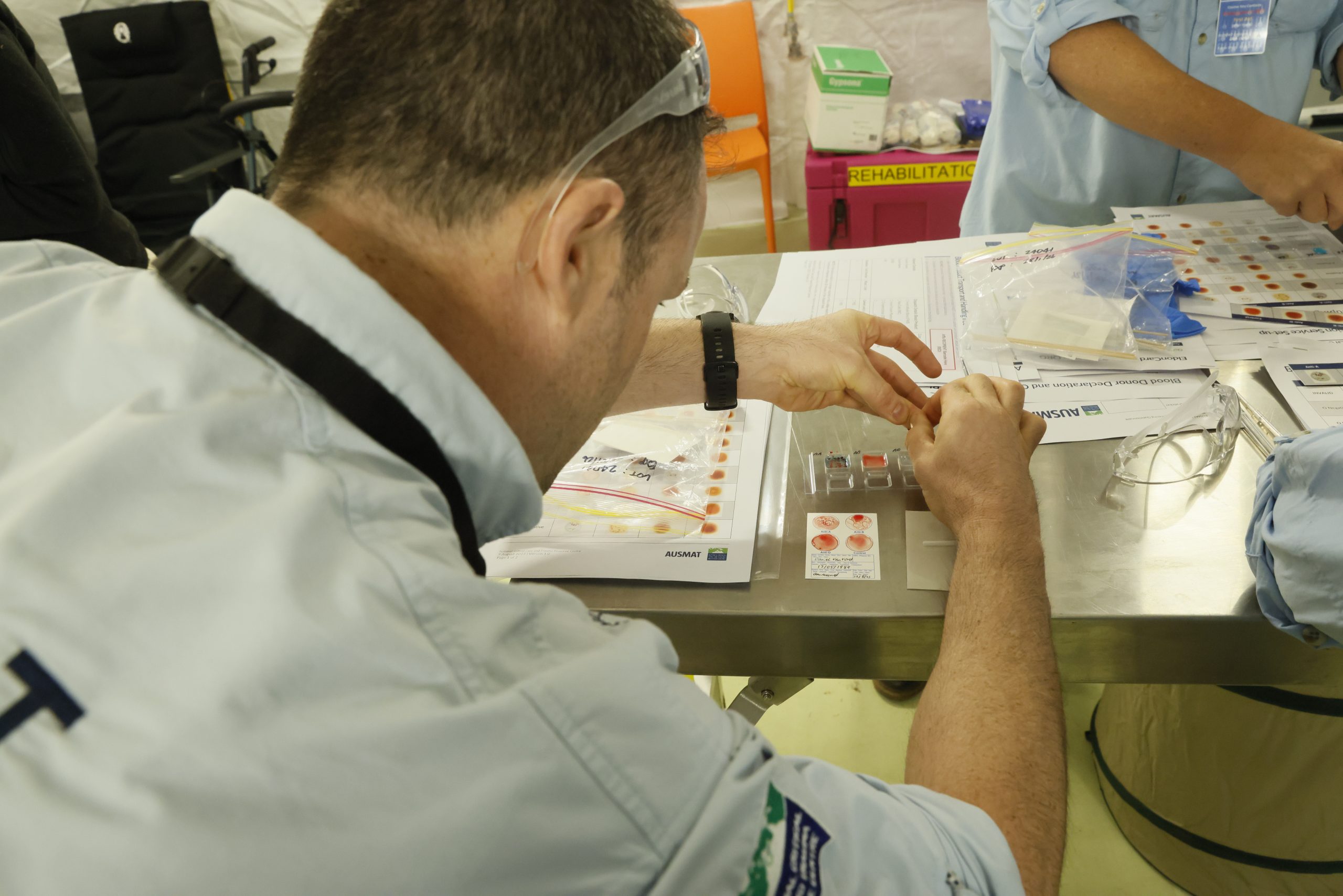
Under the guidance of AUSMAT faculty, including Leanne, participants developed the confidence needed to operate effectively in resource-limited environments. They were introduced to techniques such as whole blood transfusion, rapid blood typing using portable Eldon card test kits and blood grouping tiles, each adapted for mobile and field hospital settings. Results are available within minutes without specialised equipment, ensuring safe and timely transfusions in emergencies. These skills are critical in supporting trauma care, surgery and disaster response, where access to conventional hospital resources cannot be guaranteed.
“In hospitals we’re used to receiving pre-separated blood products,” said Clare Hayes-Bradley, anaesthetist and AUSMAT member. "Learning about whole blood transfusion helped me understand the realities of field settings."

The training also simulated donor centre workflows, equipping participants to manage blood collection and donor communication during deployments.
Stephanie Watt, a registered nurse that has been an AUSMAT member since 2023 said: “The blood grouping session was fantastic. It turned theory into practice and built my confidence to support and explain the process to potential donors.”
Dr Jerome Vili, general surgeon with the Samoan Medical Assistance Team (SEMAT), found the experience eye-opening. “Usually, as a doctor, I order blood and the lab handles the rest. This training showed me what’s involved and gave me the confidence to manage it myself if needed on deployment.”


Building regional capacity through collaboration
Alongside technical training, the course was a platform for regional engagement and collaboration. Supported by the NCCTRC’s Regional Engagement Program, Pacific EMTs exchanged insights with their Australian counterparts, building relationships to support future joint deployments.
“Training with teams like AUSMAT gives us a chance to learn from each other,” said Dr Vili. “It will help SEMAT strengthen our disaster response systems.”
Focusing on blood work was a deliberate choice in the course curriculum. Leanne explained, “The Transfusion in the field session and blood group practical are about learning technical skills and building a shared understanding of safe transfusion practices.”
The exchange of knowledge, ideas and experiences not only strengthens individual practice but also enhances the broader systems participants contribute to across the region.
Simulations that mirror reality
Participants were challenged in high pressure simulations, including managing a patient with abdominal trauma using only available field resources. These exercises tested not only clinical skills but also teamwork and communication – vital components of emergency response.
Dr Vili recalls, “We had to act with what we had – no outside help. It was stressful and it felt real. The simulation pushed me to think critically and work effectively with my team.”
Communication and teamwork were recurring themes throughout the course. “Clear communication is critical, especially in high-pressure environments,” Stephanie reflects. “The simulations tied everything together — it felt real and tested how we communicate and make decisions under pressure as a team.”
Shared training initiatives like the AUSMAT Surgical Team Member Course are essential to collective readiness, helping countries prepare together for disasters and health emergencies. Funded by the Australian Government, the course gave participants the opportunity to strengthen their clinical capabilities and build relationships that will support future deployments. After all, deployment is not the time for diplomacy or introductions.
Reflecting on the program, Course Director Associate Professor David Read, Senior AUSMAT member highlighted its broader value: Courses like this help us prepare as a region, not just as individual teams. It’s about learning, adapting and preparing together.